Surah Yunus, Ayah 9
“Indeed, those who have believed and done righteous deeds – their Lord will guide them because of their faith. Beneath them rivers will flow in the Gardens of Pleasure.”
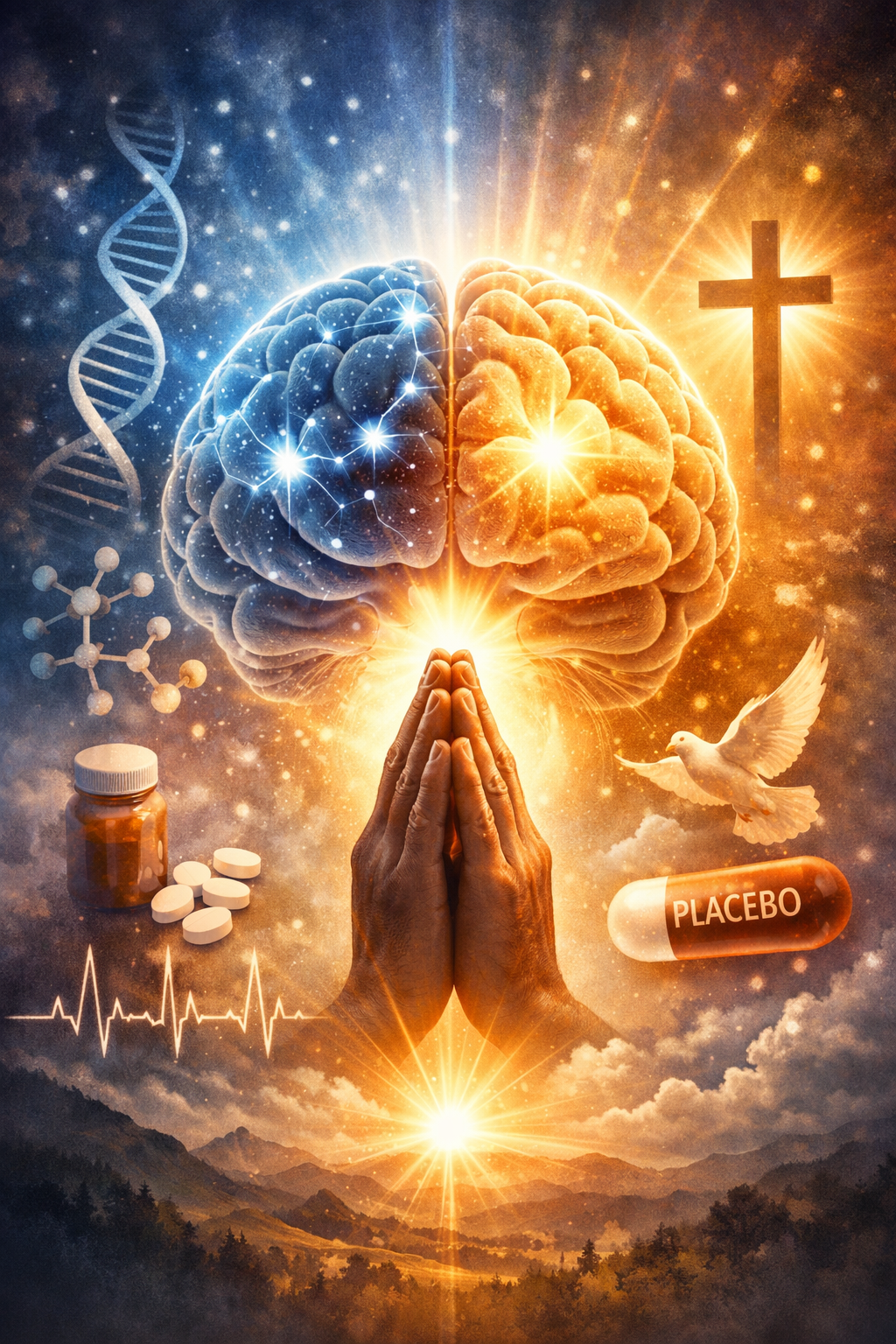
What Heals Before Medicine Arrives
On a winter morning in the early 1950s, a man named Mr. Wright lay in a hospital bed dying of cancer. His lungs were riddled with tumors; doctors had quietly prepared his family for the end. Then Wright heard about a new experimental drug—a breakthrough, whispered about in corridors. He begged for it. His physician, skeptical but compassionate, administered the injection. Within days, Wright’s tumors began to shrink. His breathing eased. X-rays improved. He walked the halls again.
Weeks later, a medical journal revealed the truth: the drug was ineffective. When Wright learned this, his symptoms returned almost immediately, and he died shortly thereafter.
Nothing “magical” was injected into his veins. Something far stranger happened instead. His brain changed his body.
————————
The Brain as a Pharmacist
Modern neuroscience no longer treats stories like Wright’s as curiosities or flukes. They are data points. The placebo effect is not imaginary, and it is not merely psychological. It is biological.
When a person expects healing, the brain does not sit passively and wait. It acts.
Functional brain imaging shows that belief activates real biochemical pathways. Expectation triggers the release of endogenous opioids (the body’s own morphine), dopamine (a motivation and reward molecule), cannabinoids (pain and stress modulators), and even serotonin. These chemicals alter pain perception, immune signaling, inflammation, heart rate, and hormonal balance.
In plain terms, the brain dispenses medicine.
This is why placebo analgesia can be blocked by naloxone, a drug that inhibits opioid receptors. When naloxone cancels a placebo’s pain relief, it proves something crucial: the relief was chemically real, not imagined.
The brain is not pretending to heal. It is healing.
Hope as a Biological Signal
Hope is often spoken of as a virtue or a mindset, but biologically, it functions as a signal. Hope tells the nervous system that the future is survivable. That signal cascades downward.
Stress biology offers a clear contrast. Chronic fear activates the hypothalamic–pituitary–adrenal axis, flooding the body with cortisol. Over time, this suppresses immune function, impairs wound healing, raises blood sugar, and accelerates aging.
Hope does the opposite. It quiets threat circuits and allows restorative systems to dominate. Parasympathetic activity increases. Heart rate variability improves. Immune cells become more responsive. Inflammation decreases.
From an evolutionary perspective, this makes sense. An organism that perceives survival as possible conserves and repairs. One that perceives doom reallocates energy to emergency responses.
Hope is not naïve optimism. It is a physiological permission slip to heal.
————————
Prayer as a Neurobiological Technology of Hope
For believers, prayer is not passive wishing. It is an active cognitive and emotional state that organizes attention, meaning, and expectation. Neuroscience increasingly suggests that prayer functions as one of the most powerful natural generators of hope the human brain possesses.
When a person prays, several things happen simultaneously. Attention narrows. Rumination quiets. Emotional regulation improves. The mind shifts from threat to trust. This shift is not abstract. Brain imaging studies of prayer and meditation show decreased activity in fear-related circuits and increased coherence in regions involved in self-regulation and emotional integration.
Prayer also supplies something medicine often lacks: a narrative of safety. To believe one is held by a higher order, watched over, or meaningful beyond the immediate crisis reduces existential uncertainty. The nervous system responds accordingly. Stress hormones fall. Parasympathetic activity rises. Immune signaling improves.
In this sense, prayer is not separate from placebo biology. It is a culturally refined, deeply conditioned form of it.
Why Belief Matters More Than Words
Not all prayer heals, just as not all placebos work. The determining factor is belief. A prayer spoken without conviction has little biological force. A prayer embedded in a lifetime of meaning, trust, and expectation can be profoundly potent.
This explains why prayer studies often yield mixed results. Prayer cannot be standardized like a pill. It depends on internal state, emotional resonance, and prior conditioning. For a true believer, prayer activates the same expectancy networks that drive placebo responses, but often more strongly, because the source of hope is perceived as absolute rather than provisional.
To the brain, certainty is chemistry.
For those who believe in miracles, prayer aligns expectation with identity. Healing is no longer something hoped for; it becomes something anticipated. That anticipation recruits the brain’s full pharmacological arsenal.
Miracles Revisited, Without Disenchantment
From this perspective, miracles do not disappear under scientific light. They relocate.
What is called a miracle may be the rare convergence of unwavering belief, emotional surrender, physiological readiness, and meaning so coherent that the body reorganizes itself around survival and repair.
Science does not yet know the limits of this reorganization. We know belief can reduce pain, modulate immunity, alter inflammation, and reshape perception. We do not yet know how far these effects can scale under optimal conditions.
Calling this “just placebo” misses the point. Placebo is the scientific name for belief becoming biology.
The Brain, Faith, and the Future of Healing
Prayer illustrates something essential: the brain does not distinguish between “spiritual” and “biological” inputs. It distinguishes between threat and safety, despair and possibility, meaninglessness and purpose.
Faith, for those who hold it, supplies an unusually stable form of purpose. That stability may be why believing minds sometimes heal where others do not. It is not that believers are immune to disease. It is that their nervous systems receive a clearer signal to fight.
As neuroscience advances, and as computational tools grow powerful enough to model layered brain-body interactions, prayer may one day be understood not as superstition, but as an ancient technology for regulating human biology through meaning.
Until then, the evidence already allows a simple, grounded conclusion:
Hope heals.
Prayer creates hope.
Belief turns hope into biology.
That is not mysticism.
It is the frontier where neuroscience, psychology, and the deepest human instincts quietly meet.
The Nocebo: When Belief Harms
The dark twin of placebo is the nocebo effect. If expectation can heal, it can also injure.
Patients told that a harmless pill may cause nausea often experience nausea. Those warned extensively about side effects report them at dramatically higher rates. In extreme cases, negative expectations can worsen pain, raise blood pressure, and suppress immune responses.
Brain imaging reveals that nocebo responses activate regions associated with anxiety and threat, amplifying pain pathways rather than dampening them. Cholecystokinin, a peptide linked to anxiety, plays a central role here.
The lesson is unsettling but empowering: the brain believes what it is told, especially by authority figures, and then recruits the body to make that belief real.
Words become chemistry.
Beyond “Just Placebo”
Critics often dismiss placebo effects with a wave of the hand: “It’s just placebo.” That phrase misses the point entirely.
If belief reliably alters physiology, then belief is a causal mechanism, not a nuisance variable. Medicine traditionally treats placebo as noise to be subtracted so that “real” drugs can shine. But neuroscience suggests the opposite framing: placebo reveals the body’s intrinsic healing architecture.
Drugs do not replace this architecture. They ride on top of it.
In fact, studies repeatedly show that the same medication works better when patients believe in it and worse when they do not. Expectation and pharmacology are not competitors. They are collaborators.
Layer Upon Layer: Why the Brain Is Still a Mystery
The human brain contains roughly 86 billion neurons, each forming thousands of connections. But neurons are only one layer. Beneath them are glial cells, vascular networks, immune cells, oscillating electrical rhythms, and molecular signaling systems that blur the boundary between mind and body.
Placebo responses appear to operate across all these layers. They involve conscious expectation, unconscious conditioning, memory, emotion, and autonomic regulation simultaneously. This is why simple explanations fail.
We are not dealing with a single “belief center.” We are dealing with a distributed system that integrates meaning into matter.
Modern tools—high-resolution brain imaging, optogenetics, machine learning models of neural networks—are only beginning to map this complexity. Future tools, possibly including quantum-enhanced computing, may help simulate and analyze the vast combinatorial states of brain activity that underlie belief-driven healing.
If that happens, placebo will stop being a footnote and become a foundation.
Are Miracles Just Biology We Don’t Understand Yet?
What people call miracles often share common features: sudden recovery, strong belief, emotional catharsis, a trusted authority, and a compelling narrative of hope. From a neuroscientific perspective, these are precisely the conditions that maximize endogenous healing responses.
This does not make such events trivial. It makes them profound.
A miracle, in this light, is not a violation of natural law. It is a moment when deeply layered biological systems align in an unusually powerful way.
Magic fades when explained, but wonder does not have to.
The Iceberg Beneath Medicine
Pharmacology has given humanity extraordinary tools. Antibiotics, vaccines, insulin, anesthesia—these are triumphs beyond debate. But beneath them lies a vast, largely untapped resource: the brain’s capacity to modulate the body.
Modern medicine has treated this capacity cautiously, even suspiciously, because it resists standardization. Belief is personal. Meaning is contextual. Hope cannot be bottled.
Yet ignoring this domain does not make it disappear. It merely leaves power unused.
The brain is not only a calculator or a storyteller. It is a chemist, an immunologist, and a systems engineer. Every thought is an intervention, whether we acknowledge it or not.
We are still at the shoreline of this understanding, looking out at an ocean of complexity. The iceberg beneath placebo is immense.
The future of healing may not lie in choosing between medicine and mind, but in finally admitting what the evidence has been whispering all along: the most sophisticated pharmacy on Earth has been inside us the whole time.
Below is a carefully curated, science-grounded reference list that supports the essay’s claims on placebo, nocebo, hope, prayer, belief, and brain-driven healing, formatted in APA 7th edition style. These are widely cited, credible sources spanning neuroscience, psychoneuroimmunology, and clinical medicine.
————————
References
Benedetti, F. (2014). Placebo effects: Understanding the mechanisms in health and disease (2nd ed.). Oxford University Press.
→ Foundational work explaining how expectations trigger endogenous opioids, dopamine, and other neurochemical pathways.
Benedetti, F., Carlino, E., & Pollo, A. (2011). How placebos change the patient’s brain. Neuropsychopharmacology, 36(1), 339–354. https://doi.org/10.1038/npp.2010.81
→ Demonstrates that placebo effects are mediated by measurable brain activity and neurotransmitter release.
Colloca, L., & Barsky, A. J. (2020). Placebo and nocebo effects. New England Journal of Medicine, 382(6), 554–561. https://doi.org/10.1056/NEJMra1907805
→ Authoritative clinical review on how expectations improve or worsen outcomes.
Kaptchuk, T. J., & Miller, F. G. (2015). Placebo effects in medicine. New England Journal of Medicine, 373(1), 8–9. https://doi.org/10.1056/NEJMp1504023
→ Reframes placebo as a meaningful component of healing rather than a nuisance variable.
Fields, H. (2018). How expectations influence pain. Pain, 159(S1), S3–S10. https://doi.org/10.1097/j.pain.0000000000001272
→ Explains how belief alters pain processing at the neural level.
Sapolsky, R. M. (2004). Why zebras don’t get ulcers (3rd ed.). Henry Holt.
→ Classic explanation of stress biology, cortisol, and how hope and safety signals protect health.
McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Reviews, 87(3), 873–904. https://doi.org/10.1152/physrev.00041.2006
→ Shows how psychological states regulate immune, metabolic, and cardiovascular systems.
Koenig, H. G. (2012). Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry, 2012, Article 278730. https://doi.org/10.5402/2012/278730
→ Reviews evidence linking prayer and religious belief to improved health outcomes.
Benson, H., & Proctor, W. (2010). Relaxation revolution. Scribner.
→ Introduces the “relaxation response,” a physiological counterpart to stress activated by prayer and meditation.
Pargament, K. I. (1997). The psychology of religion and coping. Guilford Press.
→ Explains how faith and prayer function as coping mechanisms that shape emotional and biological responses.
Wager, T. D., & Atlas, L. Y. (2015). The neuroscience of placebo effects. Trends in Cognitive Sciences, 19(5), 285–295. https://doi.org/10.1016/j.tics.2015.02.005
→ Maps placebo effects across brain networks rather than a single “belief center.”
Montgomery, G. H., Kirsch, I., & Redd, W. H. (1996). Expectancy and the placebo effect in cancer treatment. Annals of Behavioral Medicine, 18(1), 1–9. https://doi.org/10.1007/BF02893809
How expectancy influences symptom burden and treatment response in cancer patients.
Decades of neuroscience and clinical research now show that hope, expectation, and belief activate measurable brain-body pathways involving endogenous opioids, dopamine, immune signaling, and stress regulation (Benedetti, 2014; Colloca & Barsky, 2020; Wager & Atlas, 2015).”
Discover more from RETHINK! SEEK THE BRIGHT SIDE
Subscribe to get the latest posts sent to your email.