Disclaimer: The following content is for educational purposes, for health issues seek medical advice from your physician
Cholesterol is a word that often comes up in conversations about diet and heart health. It has a reputation for being bad, yet our bodies actually need cholesterol to function. So, what is cholesterol? How does our body get it and use it? Why do we hear about “good” and “bad” cholesterol? And what does current science say about managing cholesterol for health? This article will delve into the full story of cholesterol – explaining its chemical nature, its crucial roles in the body, the differences between cholesterol and the lipoproteins that carry it in our blood, and why balancing cholesterol is so important for our health.
What Is Cholesterol?
Cholesterol is a waxy, fat-like substance found in every cell of the human body . Chemically, it belongs to a class of molecules called sterols, which are a type of lipid (fat). A cholesterol molecule has a distinctive structure made of four linked carbon rings, which makes it a lipophilic (fat-loving, water-insoluble) substance. In other words, cholesterol does not dissolve in water or blood on its own. Despite often being talked about in negative terms, cholesterol itself isn’t “bad” – in fact, it is essential for life .
Chemical structure of a cholesterol molecule. Cholesterol is a sterol lipid composed of four hydrocarbon rings, making it waxy and insoluble in water. Its structure underlies its role in cell membranes and hormone production.
Chemical structure of a cholesterol molecule. Cholesterol is a sterol lipid composed of four hydrocarbon rings, making it waxy and insoluble in water. Its structure underlies its role in cell membranes and hormone production.
Being a lipid, cholesterol is similar to fats but serves different purposes. Unlike fats (such as triglycerides) that store energy, cholesterol is not a significant energy source for the body. Instead, it is a crucial building block for cells and biochemicals. It’s often described as waxy or whitish-yellow in appearance , and in the body it is mostly found tucked into cell membranes or packaged in carrier particles in the blood. Cholesterol is present only in animal-based foods (like egg yolks, meat, and cheese) and is naturally absent in plant-based foods, since plants have their own sterols (e.g. sitosterol). Our bodies, however, can make all the cholesterol we need on their own .
One common point of confusion is the difference between cholesterol and lipoproteins. Cholesterol is a single kind of molecule – a sterol lipid. Lipoproteins, on the other hand, are the particles that transport cholesterol (and other fats) through the bloodstream. We often hear terms like “LDL cholesterol” or “HDL cholesterol,” but it’s important to realize that LDL and HDL are not themselves cholesterol; they are lipoprotein particles that carry cholesterol. We’ll explore these carriers in detail later, but keep in mind that whenever we refer to “cholesterol levels” in blood, we’re usually talking about the amount of cholesterol contained in different lipoprotein particles.
How Your Body Makes Cholesterol

Cholesterol can come from two sources: your diet and your body’s own production. However, the majority of cholesterol in your body does not actually come from food. Only about 20% of the cholesterol in your bloodstream comes from the food you eat – your body makes the other 80% itself . In other words, even if you don’t eat much cholesterol, your liver and other organs will produce what you need. The liver is the primary organ responsible for cholesterol synthesis (manufacturing), using building blocks from fats, sugars, and proteins . In fact, cholesterol production is so important that if you consume less cholesterol, your body will generally ramp up its own synthesis to compensate, and vice versa .
Cholesterol is produced inside cells through a complex biochemical pathway (the mevalonate pathway), which involves many steps and enzymes. The liver plays a central role in this process and makes a significant portion of the body’s cholesterol, which it then releases into the blood. Other organs like the intestines and even individual cells throughout the body can also synthesize cholesterol as needed . Because every cell membrane needs cholesterol, most cells have the ability to make some of it. This built-in production system ensures that vital tissues (including the brain, which has a high cholesterol content) always have a supply, even if dietary intake is low.
Your body’s regulation of cholesterol production is quite sophisticated. When you eat foods high in cholesterol (like eggs or shrimp), your liver may sense the increased levels and produce less on its own. Conversely, on a low-cholesterol diet, the liver makes more. To give a sense of scale: if you eat an egg with about 200 mg of cholesterol, your liver might make several times that amount in a day to meet the body’s total needs . This is why dietary cholesterol has a more limited effect on blood cholesterol levels than one might expect – the body adjusts its own production to keep balance. (We’ll discuss later how modern guidelines view dietary cholesterol.)
Why Your Body Needs Cholesterol (Essential Functions)
Cholesterol often gets cast as a villain, but it actually performs indispensable roles in our physiology. It might help to think of cholesterol as a kind of structural “brick” and biochemical “starter material” that the body uses in many ways:

- Cell Membrane Structure: Cholesterol is a fundamental component of cell membranes in animals. If you zoom in on any cell’s outer membrane, you’ll find cholesterol nestled among the phospholipid molecules. Cholesterol helps maintain the structural integrity of the membrane and modulates its fluidity . This means cholesterol ensures that cell membranes are not too rigid but also not too flimsy. Proper membrane fluidity is crucial for cells to function – it affects how cells communicate and how substances move in and out. Without cholesterol, cell membranes would be too permeable and fragile .
- Hormone Synthesis: Cholesterol is the building block for steroid hormones. Your body converts cholesterol into vital hormones such as cortisol and aldosterone (hormones from the adrenal gland), and the sex hormones testosterone, estrogen, and progesterone . These hormones regulate critical functions from metabolism and immune response to salt balance and reproductive processes. In fact, all steroid hormones in the body (as well as vitamin D) are made by chemical modifications of the cholesterol molecule .
- Vitamin D Production: When sunlight hits your skin, it triggers a process that converts a form of cholesterol into vitamin D. So cholesterol is a direct precursor to vitamin D, which is essential for bone health and immune function .
- Bile Acid Production: Cholesterol is also used to make bile acids (or bile salts) in the liver . Bile acids are released into the intestines to help digest fats and fat-soluble vitamins (A, D, E, K). Without enough cholesterol, your body couldn’t produce the bile it needs to absorb dietary fats properly.
In short, cholesterol is essential for life . It’s woven into the fabric of our biology, from every cell wall to the production of critical hormones and nutrients. Problems arise not because cholesterol itself is evil, but because having too much cholesterol (especially in the wrong place, like in the bloodstream or artery walls) can lead to disease. It’s a delicate balance – we need cholesterol, but we need it in the right amounts and locations.
How Cholesterol Travels in the Blood (Lipoproteins vs. Cholesterol)

Because cholesterol is a fatty, waxy substance, it does not mix with water-based fluids like blood. Transporting cholesterol around the body is a bit like trying to mix oil with water – if released directly into the blood, cholesterol would clump together in globs (imagine bacon fat solidifying in a pot of water) . To solve this, the body packages cholesterol into lipoproteins for transit. Lipoproteins are tiny spherical particles made of fats (lipids) and proteins that are designed to be water-compatible carriers . Think of lipoproteins as vehicles or “boats” that ferry cholesterol (and other fats like triglycerides) through the bloodstream.
Each lipoprotein particle has an outer shell of proteins (called apolipoproteins) and phospholipids that makes it soluble in blood, and an inner core that can carry cholesterol and triglycerides safely. This structure allows cholesterol to travel to all the cells that need it . Without lipoproteins, cholesterol would simply stick to artery walls or form unusable deposits.
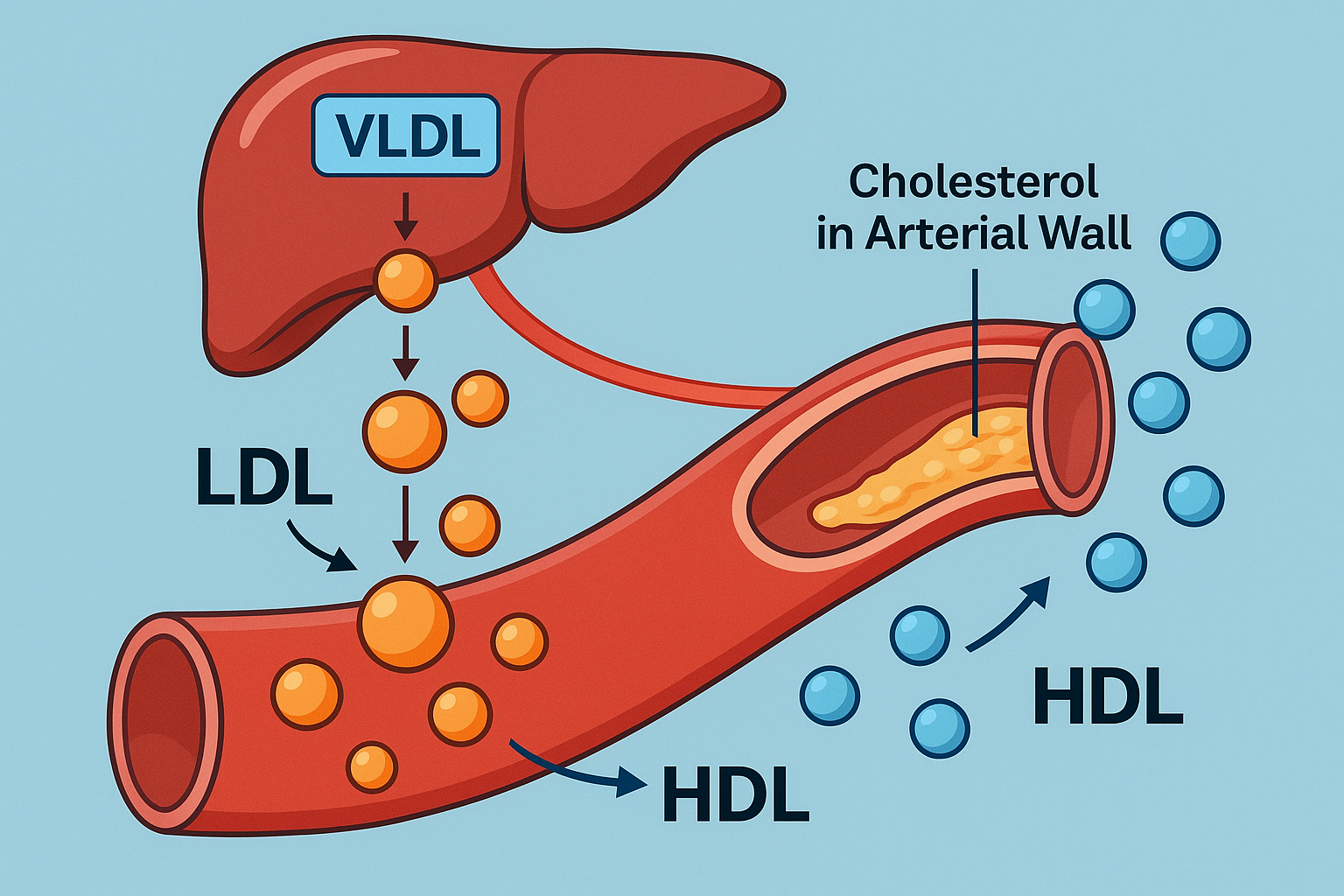
There are several types of lipoproteins, classified by their density (which reflects their fat-to-protein ratio). The main types are chylomicrons, VLDL (very-low-density lipoprotein), IDL (intermediate-density lipoprotein), LDL (low-density lipoprotein), and HDL (high-density lipoprotein) . Each type has a different job:
- Chylomicrons: These are the largest lipoproteins and carry fat from the food you eat (mostly triglycerides) from the intestine to the liver and other tissues. They are formed after a meal in your digestive tract .
- VLDL: Made by the liver, VLDL particles carry triglycerides to tissues. As tissues absorb the fat from VLDL, these particles shrink and become IDL .
- IDL: These are transitional particles formed from VLDL after delivering triglycerides. Some IDL is taken up by the liver, and the rest continues to lose triglycerides and becomes LDL .
- LDL: These particles are what’s left after VLDL/IDL have delivered most of their fat – they are now cholesterol-rich. LDL’s main job is to deliver cholesterol to cells throughout the body. Because LDL carries a high load of cholesterol, it’s the primary carrier of cholesterol in the blood .
- HDL: These particles are dense and protein-rich. HDL is like a cholesterol scavenger – it picks up excess cholesterol from the bloodstream and from artery walls and carries it back to the liver for recycling or excretion .
In summary, cholesterol is the cargo, and lipoproteins are the ships. This distinction is important: when we measure “blood cholesterol,” we are usually measuring how much cholesterol is carried by LDL, HDL, etc., not free-floating cholesterol (since virtually none is free-floating). Now, among these carrier ships, LDL and HDL are the most talked-about because of their influence on health.
Types of Cholesterol: LDL and HDL
Healthcare providers often classify cholesterol as “bad” or “good” based on whether it’s carried by LDL or HDL particles. Let’s unpack these terms:
- LDL (Low-Density Lipoprotein): Commonly known as “bad cholesterol,” LDL is the primary carrier of cholesterol to tissues. In fact, LDL particles carry roughly two-thirds of the cholesterol in circulation on average . LDL’s job is to deliver cholesterol to cells that need it for membranes, hormone production, etc. However, if there is more cholesterol (and LDL) than the body needs, this excess can deposit in artery walls (we’ll discuss how in the next section). High levels of LDL cholesterol in the blood are associated with a higher risk of cardiovascular disease . Because LDL contributes to plaque buildup in arteries, we label it “bad” when it’s elevated.
- HDL (High-Density Lipoprotein): Often called “good cholesterol,” HDL has almost the opposite role of LDL. HDL particles act as cholesterol cleaners – they absorb excess cholesterol from body tissues and artery walls and carry it back to the liver . The liver can then use that cholesterol to make bile acids or repurpose it, or it can eliminate it from the body through bile. High levels of HDL cholesterol are associated with a lower risk of heart disease and stroke . Essentially, HDL helps remove cholesterol from places where it might cause harm. It’s “good” because it fights the buildup of plaque by retrieving cholesterol from the arteries.
It’s worth noting that the cholesterol carried in LDL and HDL is the same molecule – cholesterol is cholesterol, chemically speaking. The difference lies in the carrier and the direction of transport. LDL is delivering cholesterol to the body (which is necessary, but too much delivery to arteries is harmful), whereas HDL is retrieving cholesterol and taking it out of circulation. You can think of LDL as a dump truck delivering cargo to construction sites, and HDL as a cleanup crew picking up excess debris. You need both functions; you just don’t want too much delivery without cleanup.
Aside from LDL and HDL, you may hear about VLDL and IDL in blood tests, or a calculated value called “non-HDL cholesterol” (which is basically total cholesterol minus HDL, representing all the “bad” carriers combined). VLDL and IDL are also considered contributors to artery plaque (sometimes VLDL is termed a “bad” cholesterol too), mainly because they are precursors to LDL and carry fats that can ultimately contribute to plaque . However, when it comes to health risk and guidelines, LDL and HDL are the stars of the show, with LDL being the primary target for therapy in most cases.
Why Is LDL “Bad” and HDL “Good”?
LDL and HDL have earned their nicknames through their impact on atherosclerosis, the process that underlies most heart attacks and strokes. Atherosclerosis is the buildup of fatty plaques in the walls of arteries, causing them to narrow and harden. Cholesterol – carried by LDL particles – is a major ingredient in these plaques .
Illustration of an artery with plaque buildup (cholesterol deposits). Excess LDL (“bad” cholesterol) leads to plaque formation that narrows arteries (atherosclerosis), increasing the risk of heart attacks and strokes . HDL (“good” cholesterol) helps remove cholesterol from plaques, slowing or reversing this process.
Illustration of an artery with plaque buildup (cholesterol deposits). Excess LDL (“bad” cholesterol) leads to plaque formation that narrows arteries (atherosclerosis), increasing the risk of heart attacks and strokes . HDL (“good” cholesterol) helps remove cholesterol from plaques, slowing or reversing this process.
Here’s why LDL is considered “bad” in excess: When there is too much LDL in the blood, cholesterol can start to infiltrate the artery wall. The process often begins with some damage or inflammation in the arterial lining. LDL particles slip into the artery wall and deposit cholesterol there. The immune system sees these deposits and sends in white blood cells (macrophages) to engulf the cholesterol-filled LDL – these cells become bloated “foam cells.” Over time, more and more cholesterol and cells accumulate, forming a plaque . The plaque is basically a mix of fats (including cholesterol), cells, and scar tissue that protrudes into the artery space . As plaques grow, they narrow the arteries, restricting blood flow. Even more dangerously, plaques can become unstable and rupture, causing a blood clot to form. If a clot blocks an artery in the heart or brain, it causes a heart attack or stroke. This whole cascade is fueled in large part by LDL cholesterol – the more LDL in the blood, the more cholesterol tends to deposit in arteries, accelerating plaque formation . That’s why high LDL levels raise the risk of heart disease and stroke .
On the flip side, HDL is “good” because it helps counteract this process. HDL particles patrol the bloodstream, picking up excess cholesterol, including cholesterol from those developing plaques. HDL then carries cholesterol back to the liver. The liver can package the excess cholesterol into bile and ultimately excrete it via the digestive tract. This process is known as reverse cholesterol transport – it’s essentially plaque cleanup. Higher levels of HDL cholesterol have been correlated with lower risk of heart disease in population studies, presumably because HDL is doing a good job removing cholesterol before it causes trouble .
It’s important to mention that while high HDL levels correlate with better heart health, simply raising HDL with medications has not proven to reduce heart attacks. In fact, recent clinical trials that tried to raise HDL (for example, with certain drugs) did not show the expected benefits . It appears that HDL’s protective effect is complex and not just about the amount of HDL, but how well it functions. Nonetheless, having a naturally higher HDL or improving HDL through lifestyle (exercise, for instance) is generally seen as positive for cardiovascular health.
In summary, LDL is “bad” mainly because too much of it leads to cholesterol buildup in arteries, fueling atherosclerosis . HDL is “good” because it helps remove cholesterol from arteries, acting as a safeguard. Modern medical advice centers on lowering LDL as a key strategy to reduce cardiovascular risk, while maintaining a healthy level of HDL through lifestyle.
Cholesterol vs. Lipoproteins: Understanding the Difference
By now, it’s hopefully clear that when people talk about HDL or LDL cholesterol, they’re talking about cholesterol within lipoproteins. To reinforce the distinction: cholesterol is a molecule, whereas HDL and LDL are particles (made of cholesterol, fats, and proteins) that carry that molecule. The cholesterol found inside LDL versus HDL is identical – there isn’t a “bad” form of the cholesterol molecule versus a “good” form. The goodness or badness comes from how and where cholesterol is being transported.
Another key difference is that cholesterol can’t move through blood on its own, whereas lipoproteins are built for travel. Imagine cholesterol as cargo that is greasy and water-insoluble; lipoproteins are like shipping containers that allow this greasy cargo to hitch a ride in the blood. Each lipoprotein has identifying proteins on its surface (apolipoproteins like ApoB on LDL and ApoA1 on HDL) which determine how cells recognize and handle them. For instance, cells in the liver have receptors that specifically bind to ApoB on LDL to remove LDL from circulation – this is how the liver knows to uptake LDL and thus clear cholesterol from the blood. In conditions like familial hypercholesterolemia (a genetic disorder), the LDL receptors don’t work properly, so LDL stays in the blood too long and cholesterol levels skyrocket, leading to early plaque buildup.
In everyday terminology and blood test reports, we often simplify by saying “cholesterol” when we actually mean “cholesterol within a certain type of lipoprotein.” For example, a lab report might list LDL-C and HDL-C – these are the concentrations of cholesterol carried by LDL and HDL, respectively. Understanding this nuance can clarify why, for example, one cannot directly label cholesterol itself as good or bad. It all depends on which “boat” it’s riding in and where it’s going.
Lastly, while triglycerides are a different type of fat, they often go hand-in-hand with cholesterol in discussion of lipoproteins. Triglycerides are carried mainly by chylomicrons and VLDL. People with high triglycerides often have low HDL and small, dense LDL – a combination that can be particularly harmful. The total picture of heart risk comes from looking at LDL, HDL, and triglycerides together, not cholesterol in isolation. But at its core, the difference between cholesterol and lipoproteins is: one is the payload, the others are the vehicles.
Cholesterol in Health and Disease: Current Insights and Guidelines
Our understanding of cholesterol and heart disease has grown over decades of research, and it continues to evolve. Here are some key insights from recent scientific studies and current medical guidelines:
- High LDL is a Proven Risk Factor: Decades of epidemiology and clinical trials have firmly established that elevated LDL cholesterol causes higher risk of atherosclerotic cardiovascular disease . Recent guidelines (such as the 2018 American Heart Association/American College of Cardiology cholesterol management guideline) emphasize lowering LDL as a primary goal to reduce heart attack and stroke risk, especially for people at high risk. For example, if someone has already had a heart attack or has very high LDL (above certain thresholds like 190 mg/dL), strong cholesterol-lowering therapy (usually high-intensity statin medication) is recommended to aggressively lower LDL and prevent future events.
- The Focus on LDL Targets: Unlike older guidelines that set specific target numbers for LDL (e.g., “LDL below 100 mg/dL”), newer guidelines focus more on overall risk and using appropriate intensity of therapy. The general idea is “lower is better” for LDL, especially in high-risk individuals . Some recent studies even show that very low LDL levels (achieved with powerful new drugs) can further reduce plaque and cardiovascular events, suggesting there may not be a practical lower limit in at-risk patients. However, for the general population, maintaining LDL in a healthy range (often cited as <100 mg/dL for low-risk individuals, or even lower for those with heart disease) is widely advised.
- HDL’s Complex Role: As mentioned, having a low HDL has been linked to higher heart risk, but raising HDL with drugs hasn’t yielded benefits . This was a surprising finding from trials in the 2010s. It turns out that simply having a high HDL number is not a magic shield – what matters is the function of HDL (how effectively it removes cholesterol) and the overall context of a person’s health. Nevertheless, lifestyle measures that often raise HDL – like exercise, quitting smoking, and weight loss – are beneficial for many reasons, so in practice we still encourage those. Current guidelines do not recommend any medication solely to raise HDL; instead, they focus on LDL reduction and overall healthy lifestyle for those with low HDL.
- Dietary Cholesterol vs. Blood Cholesterol: For many years, people were told to strictly limit dietary cholesterol (for example, egg yolks or shrimp) to manage blood cholesterol. However, current understanding has shifted. Research has shown that for most people, dietary cholesterol intake has a relatively modest impact on blood cholesterol levels . The 2015-2020 Dietary Guidelines for Americans removed the previous 300 mg per day cholesterol limit, though they still caution that high-cholesterol foods often come packaged with lots of saturated fat (e.g., red meat, butter) which does raise blood cholesterol. In fact, saturated and trans fats in the diet have a much bigger effect on LDL levels than dietary cholesterol does . Eating a diet high in saturated fat (found in animal fats, certain oils, and processed foods) can raise your LDL cholesterol significantly . Therefore, current guidelines (such as the American Heart Association’s recommendations) advise limiting saturated fat to help control cholesterol – often suggesting no more than about 5-7% of daily calories from saturated fat . Replacing saturated fats with unsaturated fats (like those in nuts, olive oil, fish, etc.) can improve your lipid profile.
- Lifestyle and Cholesterol: The cornerstone of managing cholesterol is still lifestyle change. A healthy diet (rich in fruits, vegetables, whole grains, lean proteins, and healthy fats), regular exercise, avoiding tobacco smoke, and maintaining a healthy weight all contribute to better cholesterol levels and lower heart risk . For instance, regular exercise can raise HDL modestly and improve how your body handles fats; quitting smoking can raise HDL and improve overall heart health; and weight loss can lower LDL and triglycerides while raising HDL. Stress management and moderation of alcohol intake (excess alcohol can raise triglycerides and add calories) also play a role.
- When Lifestyle Isn’t Enough – Medications: If lifestyle measures aren’t sufficient to get cholesterol under control (which can be the case due to genetics or very high initial levels), doctors turn to medications. The most famous class is statins, which work by reducing the liver’s cholesterol production and increasing the liver’s uptake of LDL from the blood. Statins are well-proven to reduce the risk of heart attacks and strokes and are first-line therapy for high LDL or high-risk patients . Recent years have also seen the development of new cholesterol-lowering drugs, such as PCSK9 inhibitors, which can dramatically lower LDL levels by improving the liver’s ability to remove LDL from blood. There are also other medications like ezetimibe (which blocks cholesterol absorption in the gut) and bile acid sequestrants. Current guidelines often recommend a stepped approach: start with lifestyle changes, assess risk, and if risk is high or LDL remains high, add medications to reach sufficient LDL reduction .
- Current Goals and Guidelines: For a generally healthy person, desirable blood cholesterol levels are often cited as: total cholesterol < 200 mg/dL, LDL cholesterol < 100 mg/dL, HDL cholesterol > 40 mg/dL (men) or > 50 mg/dL (women), and triglycerides < 150 mg/dL. However, targets can differ based on individual risk factors. Someone with existing heart disease or diabetes, for example, is often advised to aim for even lower LDL (sometimes < 70 mg/dL). The American Heart Association and American College of Cardiology recommend using a risk calculator to determine if a person would benefit from a statin; generally, if a person’s 10-year risk of heart attack or stroke is moderate or high, or if LDL is very high, cholesterol-lowering therapy is advised in addition to lifestyle changes.
- Emerging Research: Scientists continue to research cholesterol metabolism and its role in disease. For instance, there is interest in the role of inflammation in atherosclerosis – it’s not just about cholesterol numbers, but also about the inflammatory response to cholesterol in the arteries. Some newer therapies (like certain anti-inflammatory drugs) have been shown to reduce heart risk when added to cholesterol-lowering therapy, highlighting that heart disease is multifactorial. There is also research into genetic factors that influence cholesterol. The discovery of genetic mutations (like those in the PCSK9 gene) has opened new doors to treatments and underscored how some people’s bodies handle cholesterol differently.
In wrapping up the full story of cholesterol, the take-home message is one of balance and informed management. Cholesterol itself is a vital substance – without it, we couldn’t survive. But too much cholesterol in the bloodstream, particularly in LDL form, can lead to life-threatening diseases. HDL offers a natural counterbalance by helping remove excess cholesterol. Modern medicine, backed by research from organizations like the National Institutes of Health and the American Heart Association, encourages us to maintain healthy cholesterol levels through diet and lifestyle, and to use medications when necessary to protect against heart disease . Knowing your cholesterol numbers (via a blood test) and understanding the difference between LDL and HDL is an empowering part of taking charge of your health.
Cholesterol, in summary, is neither good nor bad on its own – it’s an essential molecule that becomes a problem only when out of balance. By eating wisely, staying active, and following medical guidance for check-ups and treatments, you can ensure that cholesterol continues to play its positive roles in your body while minimizing its potential to do harm. That’s the full story of cholesterol: a tale of chemistry, biology, and health, illustrating how something so small can have such a big impact on our lives.
Why does LDL sometimes rise too high?
Excess “bad” LDL-cholesterol almost always reflects an imbalance between how much cholesterol-rich lipoprotein the liver puts into the bloodstream (largely as VLDL that later becomes LDL) and how quickly the body clears those particles via LDL-receptors. Several overlapping forces can tip this balance.
⸻
1. Lifestyle‐driven overproduction and slowed clearance – the dominant cause
A diet rich in saturated or trans-fats, excess calories, and very low physical activity drives weight-gain and visceral (belly) fat. Visceral fat releases free-fatty-acids and inflammatory cytokines into the portal vein; the liver converts this flood of fat into more VLDL particles. Cytokines plus insulin-resistance also down-regulate LDL-receptors, so fewer LDL particles are removed from the blood. The net effect is higher circulating LDL-C. These mechanisms explain why 60-70 % of people with obesity show dyslipidaemia that includes raised LDL or increased LDL-particle number and “small-dense” LDL traits
⸻
2. Genetic set-points
In some families the LDL receptor itself is faulty (familial hypercholesterolaemia) or liver cholesterol synthesis is overactive. These inherited variants can push LDL above 190 mg/dL even in lean, very active people; lifestyle still matters, but genetics set a high baseline. (Every major guideline lists monogenic disorders as the second most common cause of high LDL after lifestyle.)
⸻
3. Chronic low-grade inflammation – a bidirectional amplifier
Your hunch is half-right: chronic, smouldering inflammation does not usually make the liver crank out “extra” LDL merely to patch damage, but it does reshape lipoprotein metabolism in ways that magnify LDL-related risk:
- Cytokines such as IL-6 and TNF-α stimulate VLDL secretion and further blunt LDL-receptor activity, nudging LDL upward, especially in people with visceral obesity or metabolic syndrome.
- Inflammatory enzymes oxidise and shrink LDL particles, turning them into small-dense LDL that linger longer in plasma and lodge more readily in artery walls
- Conversely, acute severe inflammation (e.g., sepsis) actually lowers LDL transiently, illustrating that the relationship is complex
Thus inflammation is better viewed as a co-conspirator that worsens LDL quality and clearance, rather than the primary driver of high LDL in the general population.
⸻
4. Secondary medical and drug causes
- Endocrine and metabolic conditions (hypothyroidism, uncontrolled diabetes, nephrotic syndrome) reduce LDL-receptor activity or increase VLDL secretion.
- Certain medicines (anabolic steroids, some immunosuppressants, HIV protease inhibitors) raise LDL by similar mechanisms.
- Aging and estrogen decline modestly raise LDL because hepatic LDL-receptor numbers fall over time. All of these are routinely screened when unexplained LDL elevations persist.
⸻
Putting the pieces together
For most adults, excess LDL is the metabolic fingerprint of an energy-rich, sedentary, pro-inflammatory milieu overlaid on individual genetics. Tackling the root causes—weight reduction, diets lower in saturated fat and higher in unsaturated fat, regular exercise, smoking cessation, and control of conditions such as diabetes or hypothyroidism—usually normalises LDL. When lifestyle and inflammation control do not suffice or when genetics sets LDL far above target, LDL-lowering drugs (statins first, then ezetimibe or PCSK9 inhibitors) restore the production-clearance balance and cut cardiovascular risk.
In short, inflammation modifies LDL metabolism and atherogenicity, but the chief culprit behind chronically high LDL remains an excess of hepatic lipoprotein production and impaired clearance driven by diet, adiposity, insulin-resistance, and genetics.
References:
1. MedlinePlus, Cholesterol – What is cholesterol?
2. StatPearls – Huff T. et al., Physiology, Cholesterol, NCBI Bookshelf (2023)
3. CDC – LDL and HDL Cholesterol: “Bad” and “Good” Cholesterol (May 15, 2024)
4. Harvard Health Publishing – Corliss J., How it’s made: Cholesterol production in your body (Harvard Heart Letter)
5. StatPearls – Huff T. et al., Physiology, Cholesterol – Cholesterol transport and lipoproteins
6. MedlinePlus – What are HDL, LDL, and VLDL? (U.S. National Library of Medicine)
7. StatPearls – Huff T. et al., Physiology, Cholesterol – Atherosclerosis and cholesterol
8. StatPearls – Huff T. et al., Physiology, Cholesterol – Diet, lifestyle and cholesterol
Discover more from RETHINK! SEEK THE BRIGHT SIDE
Subscribe to get the latest posts sent to your email.