The Silent Culprit: Insulin Resistance and Chronic Disease
By: Sufi brothers, Rethink Nexus
It started with a routine check-up. Maria, a 52-year-old mother of two, felt a bit more tired lately, but she blamed it on a busy life. Her doctor’s call after a blood test was a surprise: she had prediabetes and slightly elevated blood pressure. Determined to get healthier, Maria improved her diet and tried to exercise sporadically. But a year later, she woke up in a hospital bed after a mild heart attack. Shaken and confused, she learned that a silent underlying condition had been fueling her health problems for years. Her doctor explained that many of Maria’s troubles – the creeping blood sugar levels, hypertension, and even risks to her brain health – traced back to a single source: insulin resistance. This quiet metabolic glitch was the invisible thread connecting multiple chronic disorders in her life. Maria’s story, though startling, is increasingly common and highlights a medical mystery now at center stage in public health.
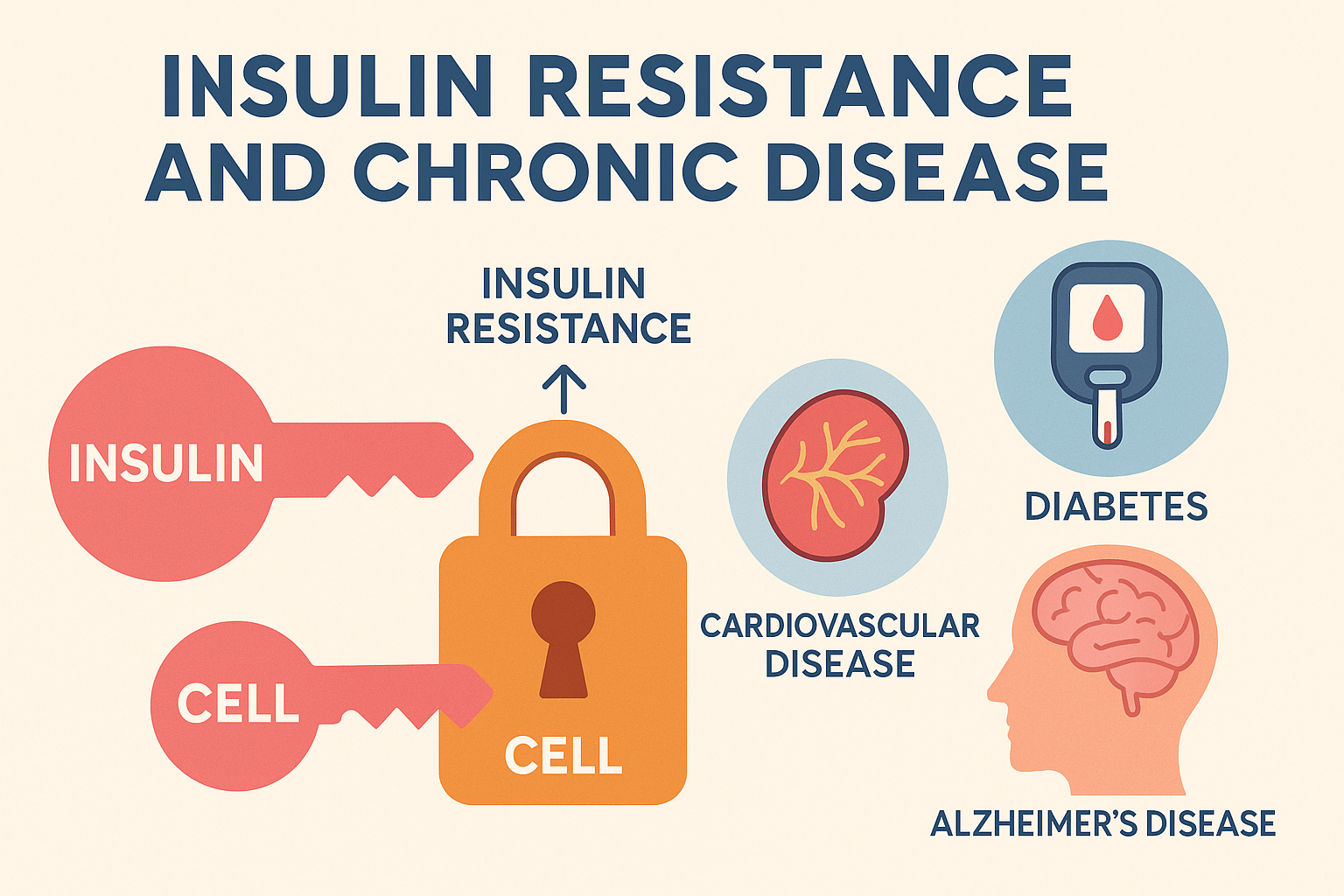
Insulin resistance (often abbreviated IR) isn’t something you can see or feel at first. It develops subtly, often over years, yet it has the power to drive conditions like type 2 diabetes, cardiovascular disease, and even Alzheimer’s disease. In this article, we will unravel how insulin resistance works and why it has such wide-reaching impact. Recent scientific findings have shed new light on this condition, and the picture is both alarming and empowering: alarming because insulin resistance is so pervasive, yet empowering because understanding it gives us tools to fight back. Before exploring its links to specific diseases, let’s start with the basics of what insulin resistance is and why it matters.
Understanding Insulin Resistance: The Body’s Silent Struggle
Insulin is a hormone best known for its role in controlling blood sugar. When we eat, our blood sugar rises and the pancreas releases insulin. This hormone is like a key, unlocking cells so they can take in glucose from the blood to use as energy. In a healthy system, this process keeps blood sugar levels in balance. Insulin resistance, however, means the body’s cells stop responding properly to insulin’s signal. It’s as if the locks on the cells have grown rusty: the key (insulin) is present, but it no longer opens the door efficiently. The result? Sugar begins to build up in the bloodstream because cells aren’t absorbing it well, and the pancreas tries to compensate by pumping out even more insulin. This state of “too much insulin, not enough effect” defines insulin resistance .
When insulin resistance first develops, it does not cause obvious symptoms. You won’t feel immediate pain or sickness. Many people, like Maria, go years without knowing their body is struggling with this issue. At most, there may be subtle signs: feeling unusually tired after meals, cravings for carbs, gaining weight around the waistline, or mildly high blood pressure and cholesterol during routine exams . These clues are often missed or attributed to aging or stress. Indeed, insulin resistance can persist silently for a decade or more until it finally progresses to more visible disorders . Doctors often discover it only when a patient develops prediabetes, type 2 diabetes, or a cardiovascular complication.
Behind the scenes, insulin resistance sets off a cascade of metabolic disturbances. Cells in key organs – the muscles, liver, and fat tissue – fail to respond to insulin, so glucose uptake is impaired. Blood sugar levels creep upward and the balance of fats in the blood is disrupted . The body’s metabolism becomes less efficient. To make matters worse, carrying excess body fat (especially around the abdomen) and a diet high in processed carbohydrates can aggravate insulin resistance, creating a vicious cycle. These factors provoke chronic low-grade inflammation, which further interferes with insulin’s signaling in cells . In other words, poor diet and inactivity, combined with genetic predisposition, feed into insulin resistance – and insulin resistance in turn feeds into worse metabolic health. Over time, this sets the stage for multiple chronic diseases.
How common is insulin resistance? Experts warn it is extremely prevalent – an unseen epidemic. Epidemiological studies estimate that in developed countries, roughly one in two adults may have some degree of insulin resistance . Many of these individuals won’t know it until serious issues arise. It’s a silent culprit lurking in the background of global health. Now, let’s shine light on how this metabolic condition drives three major chronic disorders that are on the rise: diabetes, cardiovascular disease, and Alzheimer’s disease.
Diabetes: Insulin Resistance Unmasked
It’s no coincidence that type 2 diabetes often appears after years of insulin resistance – in fact, it’s the direct consequence. Type 2 diabetes is characterized by chronically high blood sugar levels, and the principal cause is the body’s resistance to insulin. In the early stages of insulin resistance, the pancreas compensates by producing extra insulin (a condition known as hyperinsulinemia) to keep blood sugar near normal . However, this compensation cannot go on forever. After years of overwork, the insulin-producing cells begin to falter. The pancreas can no longer churn out enough insulin to overcome the resistance, and blood sugar levels begin to rise out of control . This tipping point is when prediabetes transitions to full-blown type 2 diabetes.
Type 2 diabetes has exploded in prevalence worldwide, precisely because insulin resistance has become so common. In 2025, an estimated 590 million adults around the globe are living with diabetes – about 1 in 9 people . Over 90% of those cases are type 2 diabetes , meaning they are rooted in insulin resistance. When insulin can’t do its job, glucose stays in the bloodstream, causing damage throughout the body. People with type 2 diabetes often experience fatigue, frequent urination, thirst, and unintentional weight loss, but long before these symptoms, the quiet process of insulin resistance has been at work. As Dr. Griffin Rodgers of the U.S. National Institute of Diabetes and Digestive and Kidney Diseases notes, the rise in type 2 diabetes in younger people is largely a result of the obesity epidemic and sedentary lifestyles – the same factors that drive insulin resistance.
Untreated diabetes can lead to severe complications: nerve damage, kidney failure, vision loss, and more. But it’s important to realize that insulin resistance typically precedes diabetes by many years . This offers a crucial window for prevention. By diagnosing insulin resistance or prediabetes early – and intervening with lifestyle changes – it is often possible to delay or even prevent the progression to type 2 diabetes. Indeed, large studies have shown that people with prediabetes can avoid developing diabetes by losing modest weight and increasing physical activity. Maria’s initial diagnosis of prediabetes was actually an alarm bell indicating that her cells were insulin resistant. Addressing insulin resistance at that stage is like fixing a leaky roof before the whole house is flooded.
In summary, insulin resistance is the engine behind the wheel of type 2 diabetes. It drives high blood sugar and forces the pancreas into overdrive until it burns out. Type 2 diabetes is essentially insulin resistance reaching its breaking point. Controlling this condition early on is key to stopping diabetes in its tracks – and as we’ll see, doing so pays dividends not just for diabetes itself, but for many other aspects of health.
The Heart at Risk: Insulin Resistance and Cardiovascular Disease
Long before diabetes is diagnosed, insulin resistance may already be quietly damaging the heart and blood vessels. Cardiovascular disease – which includes heart attacks, strokes, and hypertension – is another arena where insulin resistance plays a major role. In fact, researchers now recognize insulin resistance and the accompanying high insulin levels (hyperinsulinemia) as independent risk factors for heart disease, on par with better-known factors like high cholesterol and smoking . Yet this risk often goes underestimated because, unlike cholesterol or blood pressure, we don’t routinely screen for insulin resistance in the general population . The result is that many people are unaware of the cardiovascular time bomb ticking inside them.
How exactly does insulin resistance harm the cardiovascular system? Scientists have uncovered several interconnected mechanisms. First, when cells stop responding to insulin, the body compensates by flooding the bloodstream with more insulin. Chronically high insulin levels can have damaging effects on blood vessels. Under healthy conditions, insulin has a helpful role in the cardiovascular system – it stimulates the production of nitric oxide, a molecule that helps blood vessels relax and dilate. But in insulin resistance, this balance is upset. The pathway by which insulin normally supports blood vessel function is impaired, while a different insulin-triggered pathway (involving a molecule called endothelin-1) can become overactive . The result is narrowed, stiffer blood vessels – a state known as endothelial dysfunction – which is a precursor to atherosclerosis, the buildup of plaques in arteries . Essentially, insulin resistance pushes the gas pedal on processes that cause blood vessels to constrict and fosters the growth of arterial plaques.
Second, insulin resistance often goes hand-in-hand with a cluster of metabolic problems – a combination termed metabolic syndrome. This includes high blood sugar, high blood pressure, abnormal cholesterol levels, and excess abdominal fat. It’s no coincidence that all these tend to appear together; insulin resistance is a common thread weaving them into one dangerous package . Someone with insulin resistance may develop higher triglycerides and lower HDL (“good”) cholesterol, promoting plaque formation in arteries. They may also experience increases in blood pressure, partly because excess insulin tells the kidneys to retain salt and activates the sympathetic nervous system . Over time, this hypertension further damages artery walls. In Maria’s case, her slightly high blood pressure and cholesterol were early red flags of this metabolic syndrome driven by insulin resistance.
The culmination of these effects is a significantly higher risk of cardiovascular disease. Multiple studies have shown that insulin resistance is a strong predictor of atherosclerotic heart disease . Even before blood sugar reaches diabetic levels, insulin resistance is working to clog arteries and strain the heart. It’s telling that many individuals suffer a heart attack or stroke before they ever become diabetic – insulin resistance was at work, behind the scenes. Conversely, people with type 2 diabetes (who by definition have insulin resistance) are two to four times more likely to have heart disease or stroke than people without diabetes. The American Heart Association now flags insulin resistance as a key target for reducing cardiac risk.
On a hopeful note, addressing insulin resistance can improve heart health dramatically. Studies find that improving insulin sensitivity – through diet, exercise, or medications – can reduce blood pressure, improve cholesterol, and slow plaque buildup. In Maria’s story, once she understood insulin resistance was undermining her heart, she embraced changes that not only lowered her blood sugar but also eased the strain on her arteries. Her case underscores a crucial lesson: To protect our hearts, we must pay attention to insulin resistance early – not wait until it turns into diabetes or a cardiac event. The heart may truly be under threat from this “silent culprit,” but by unmasking it, we gain a powerful ally in prevention.
Alzheimer’s Disease: A New Frontier of Insulin Resistance
Perhaps the most surprising link with insulin resistance is its connection to the brain, in particular to Alzheimer’s disease. Alzheimer’s is a complex neurodegenerative disorder that causes memory loss and cognitive decline, mostly in older adults. For years, its primary hallmarks were thought to be plaques and tangles in the brain, not metabolic problems. But growing evidence now suggests that insulin resistance in the brain may be a key contributor to Alzheimer’s – so much so that some scientists have nicknamed Alzheimer’s disease “type 3 diabetes.” This nickname reflects the observation that the brains of individuals with Alzheimer’s show patterns of insulin resistance and glucose deprivation similar to a diabetic state.
Insulin is not only active in the body; it also plays important roles in the brain. In a healthy brain, insulin helps neurons regulate their metabolism and supports synaptic connections (the links between brain cells that underlie learning and memory). Insulin resistance impairs these vital brain functions. If brain cells become less responsive to insulin, they struggle to absorb glucose efficiently, leaving neurons underpowered. Research indicates that when insulin signaling in the brain falters, it can trigger the very changes that define Alzheimer’s: the accumulation of abnormal protein clumps known as beta-amyloid plaques and the formation of twisted protein fibers called tau tangles . These toxic buildups eventually kill neurons and erode memory and thinking abilities.
One striking clue linking insulin resistance to Alzheimer’s is the observation that people with type 2 diabetes have a much higher risk of developing Alzheimer’s disease than those without diabetes. Studies have found that long-term diabetes nearly doubles the risk of Alzheimer’s and other forms of dementia. Insulin resistance is believed to be a major reason for this connection . Essentially, years of insulin resistance and high blood sugar may damage brain blood vessels, promote inflammation, and directly starve neurons of energy – a triple whammy for brain health. Autopsy studies of brains from Alzheimer’s patients have shown impairments in insulin signaling pathways, suggesting a diabetic state in the brain even among some who were never diabetic in the rest of their body.
Emerging scientific findings offer hope that tackling insulin resistance might slow or prevent Alzheimer’s progression. Experimental treatments have tried approaches like delivering insulin to the brain via a nasal spray or using insulin-sensitizing medications (like those for diabetes) to improve cognition. Some small clinical trials have reported that improving insulin response in the brain can improve memory performance or at least stabilize it in people with mild Alzheimer’s. While research is ongoing and Alzheimer’s disease is multifactorial, the insulin resistance link has opened a promising new preventive angle: what’s good for blood sugar control might also be very good for the brain. Maintaining healthy insulin function through diet and exercise could, therefore, be an investment in long-term brain health.
In summary, Alzheimer’s disease appears to be another devastating outcome that insulin resistance can influence. Just as with heart disease and diabetes, the connection comes down to cells not getting the energy and signals they need because insulin’s message isn’t getting through. This area of research is fast-evolving. Scientists are now closely examining how improving insulin sensitivity might fend off neurodegeneration. The takeaway for all of us is profound: keeping insulin resistance at bay might not only lengthen our lives, but also preserve the quality of our minds as we age .
Breaking the Cycle: Preventing and Managing Insulin Resistance
The far-reaching impact of insulin resistance – from blood sugar troubles to heart disease to cognitive decline – can sound alarming. The good news is that insulin resistance is not only detectable, but also reversible, especially in its early stages. We have a growing body of knowledge about how to improve the body’s insulin sensitivity. At the core of the solution are sustainable lifestyle changes. These changes may sound simple, but they are powerful enough to potentially delay or prevent diseases in millions of people. Recent expert guidelines and studies emphasize that the same habits that prevent diabetes and heart disease also combat insulin resistance and even reduce risk for some cancers . In fact, what’s good for insulin resistance turns out to be good for overall health. Here are some practical, actionable steps individuals can take to fight insulin resistance:
- Adopt a whole-food, balanced diet: Focus on eating unprocessed or minimally processed foods – vegetables, fruits, whole grains, legumes, nuts, and lean proteins. Avoiding excess added sugars and refined carbohydrates is key, as these can spike insulin levels. Diets emphasizing whole foods, such as the Mediterranean diet or DASH diet, have been shown to improve insulin sensitivity. A healthy plate might be about two-thirds plant foods (like veggies, fruits, whole grains, beans) and one-third protein (fish, poultry, or plant protein) with healthy fats in moderation . In contrast, ultra-processed foods (sugary drinks, packaged snacks, fast foods) tend to drive insulin resistance and should be limited . Importantly, you don’t need to follow a strict fad diet – the goal is a balanced, nutritious diet that you can maintain for life.
- Lose excess weight (if needed): Weight management is perhaps the most effective way to restore insulin sensitivity. Excess visceral fat (fat around the organs and waist) is a major contributor to insulin resistance. The encouraging news is that even modest weight loss yields outsized benefits. Research shows that losing as little as 5–10% of one’s body weight can significantly lower insulin resistance and blood sugar levels . For someone weighing 200 pounds, a 10% loss is 20 pounds – a challenging but realistic target with diet and exercise. Many people find that as they shed weight, they have more energy and their blood markers (glucose, cholesterol, blood pressure) improve, reflecting better insulin action in their cells. Maintaining a healthy weight not only helps prevent type 2 diabetes but also reduces strain on the heart and might protect the brain over the long term.
- Stay physically active: Exercise is a true antidote to insulin resistance. When we exercise, our muscles can absorb glucose from the blood without requiring insulin, which gives the pancreas a well-deserved break . Regular physical activity also helps cells become more responsive to insulin when it is present. Health experts recommend at least 150 minutes of moderate exercise per week (such as brisk walking, cycling, or swimming), along with some form of strength training or resistance exercise a couple of times per week . Building lean muscle through activities like weight training is especially beneficial, since muscle tissue is very effective at using glucose. Even daily habits like taking the stairs, doing active housework, or short walk breaks during the workday can move the needle. The key is consistency – finding activities you enjoy and making movement a routine part of life. Maria, for example, started walking each morning and noticed her blood sugar readings improve within months, a direct sign that her muscles were soaking up glucose and easing the burden on insulin.
- Prioritize sleep and stress management: It may come as a surprise, but chronic lack of sleep and high stress levels can worsen insulin resistance. Poor sleep affects hormones that regulate hunger and blood sugar, often leading to weight gain and higher blood glucose. Studies have shown that even a single week of sleep deprivation can make people’s cells less sensitive to insulin. Similarly, stress triggers the release of cortisol, a hormone that can raise blood sugar and interfere with insulin’s action. Aim for 7–8 hours of quality sleep per night, and employ stress-reduction techniques that work for you – whether it’s mindfulness meditation, yoga, deep breathing, or simply enjoyable hobbies. These “rest and relax” strategies aren’t just good for mental well-being; they have tangible benefits for metabolic health, giving your body a chance to recalibrate and respond to insulin more normally.
- Regular health check-ups: Because insulin resistance develops silently, regular medical check-ups are invaluable for early detection. Doctors can assess risk factors such as fasting blood glucose, HbA1c (a measure of long-term blood sugar levels), fasting insulin levels, and cholesterol profile. If you have a family history of diabetes or early heart disease, or if you carry excess weight around your waist, it’s wise to discuss insulin resistance with your healthcare provider. In some cases, physicians may use proxy measures like HOMA-IR or triglyceride-glucose index from blood tests to gauge insulin resistance . Identifying the issue early allows for prompt intervention. Sometimes, medications like metformin (a drug that improves insulin sensitivity) are recommended for those with high risk or established diabetes – but lifestyle remains the cornerstone of management. By keeping tabs on your numbers, you and your doctor can track improvements as you make healthy changes.
These steps, while straightforward, can be life-changing. They attack insulin resistance at its root, by helping the body use insulin more effectively and reducing the load on the pancreas. It’s worth noting that improvements in insulin sensitivity can happen relatively quickly. Studies have found that changes such as cutting out sugary drinks or walking daily can improve insulin response in a matter of weeks. Of course, the goal is sustaining these habits for the long run, which in turn sustains the benefits.
Conclusion: A Unified Approach to Health
Insulin resistance may be a common thread weaving together diabetes, heart disease, Alzheimer’s, and other conditions (like fatty liver disease and polycystic ovary syndrome, to name a few), but this common enemy also presents a common opportunity. By tackling insulin resistance, we address multiple chronic diseases in one effort. The latest scientific understanding reinforces an empowering message: the way we eat, move, sleep, and manage stress today can profoundly shape our health tomorrow.
Maria’s ordeal had a silver lining. Once she learned that insulin resistance was at the core of her health problems, she took charge of her lifestyle with newfound determination. She lost weight with a balanced diet, kept up her daily walks, and practiced better sleep hygiene. Over time, her blood sugar fell out of the prediabetic range, her blood pressure improved, and she felt more energetic than she had in years. Perhaps most comforting, she knew she was also protecting herself against future ills that had plagued her own parents – her father’s heart disease and her mother’s memory loss.
The science is clear and compelling: insulin resistance is not an irreversible fate. It is a dynamic condition that can improve with the right interventions. In a world where chronic diseases are often viewed as separate silos, insulin resistance emerges as a unifying target – a chance to simultaneously curb the tide of diabetes, safeguard cardiovascular health, and possibly even shield our brains from decline. By recognizing this “silent culprit” early and taking action, we each have the potential to rewrite our health story for the better, one habit at a time.
References:
1. Ahn, B. (2025). Advances in Insulin Resistance—Molecular Mechanisms, Therapeutic Targets, and Future Directions. Int. J. Mol. Sci., 26(6), 2574.
2. Frontoni, S. et al. (2024). Insulin resistance/hyperinsulinemia: an important cardiovascular risk factor that has long been underestimated. Front. Cardiovasc. Med., 11, 1380506.
3. Frontoni, S. et al. (2024). Ibid.
4. Frontoni, S. et al. (2024). Ibid.
5. Abdalla, M.M.I. (2024). Insulin resistance as the molecular link between diabetes and Alzheimer’s disease. World J. Diabetes, 15(7), 1430-1447.
6. MD Anderson Cancer Center. (2023). What’s the best diet for insulin resistance? (B. Rodgers, Senior Clinical Dietitian)
7. MD Anderson Cancer Center. (2023). Ibid.
8. International Diabetes Federation. (2025). IDF Diabetes Atlas 11th Edition – Facts & Figures.